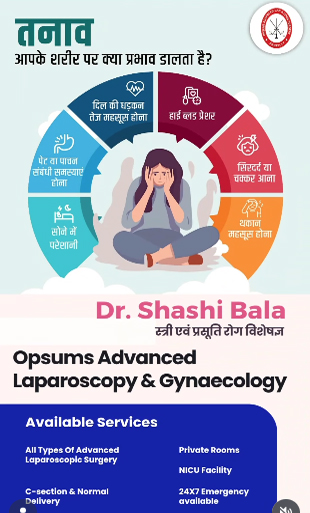
What effect does stress have on your body?
While this isn't a single case update, we are continually documenting the profound and varied effects of chronic stress on our patients’ overall health. We recognize stress as a major contributing factor in a broad spectrum of diseases, acting as a catalyst that can exacerbate existing conditions or trigger new ones.
The Systemic Impact of Stress
When the body perceives a threat, the Hypothalamic-Pituitary-Adrenal (HPA) axis is activated, leading to a cascade of physiological changes—the famous "fight or flight" response.
Our clinical observations frequently show the long-term consequences of this persistent activation:
Cardiovascular System: Sustained increases in heart rate and blood pressure, contributing to hypertension and other cardiac risks.
Immune System: Chronic high levels of cortisol can suppress immune function, making patients more susceptible to infection and slowing down healing.
Digestive System: Stress disrupts the gut-brain axis, often leading to symptoms like Irritable Bowel Syndrome (IBS) or exacerbating peptic issues.
Musculoskeletal System: Increased muscle tension often results in chronic pain, particularly in the neck and back.
Our Integrated Approach
We are increasingly integrating stress-reduction strategies into patient care plans, even when treating seemingly unrelated physical ailments. These strategies include cognitive behavioral techniques and mindful practices designed to downregulate the HPA axis.
Addressing the root cause of stress is not just about mental health—it is a critical component of treating and preventing chronic physical disease.
We continue to track the data and utilize these holistic methods to improve the resilience and long-term health outcomes of our patient population.